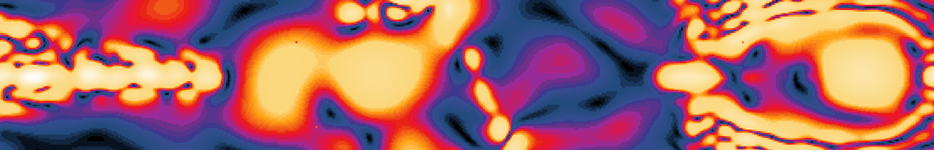

Simulation of the temperature distribution in a human body in a hyperthermia applicator.
Thermal Solvers - Tissue Heating
Background
Tissue heating and cooling is relevant in multiple areas: Temperature increase is one of the most established pathways of EM-tissue interactions and often the relevant quantity in exposure safety assessments (e.g., mobile phone safety, MR safety). Increasing tissue temperature intentionally can be therapeutically beneficial (e.g., in tumors), and very large temperature changes can be applied to ablate tissue, perform surgery, or cauterize wounds. The local and global impact of blood flow and thermoregulation must be carefully considered to assess tissue heating effects.
Selected Past Achievements
- Development of a novel perfusion model that flexibly merges discrete vessels, continuum models, tensorial effective heat conductivity, CFD, inhomogeneous perfusion maps, local and global thermoregulation, and body-core heating models to realistically consider the impact of blood flow.
- Implementation of a thermal solver to consider the above-mentioned perfusion model, environmental factors, state transitions, cell-water evaporation and rehydration by diffusion, and changes in metabolic activity. Development of novel numerical algorithms to increase the precision and speed (e.g., thin structure technique, conformal corrections, efficient parallelization and preconditioning, hardware acceleration, etc.).
- Application of the thermal solver with anatomical models to assess the MR safety of medical implants (cardiac, neural) for major implant manufacturers, to model medical treatments (hyperthermia, FUS, laser and RF/MW ablation, and RF surgery), and to study EM induced heating from mobile phones.
- Development of thermal dose- and tissue damage-based approaches to assess EM exposure safety (likely basis for new MR safety guidelines) and for applications in the real-time supervision of a new parallel transmit imaging technique.
Next Challenges
- To integrate advanced models of tissue damage-induced perfusion and tissue property changes
- To perform in vivo validations.